 Insurance companies are denying coverage for proton therapy
Insurance companies are denying coverage for proton therapytreatment that could save the lives of cancer patients. Although targeted
radiation therapy is becoming increasingly popular among oncology doctors
across the globe and it is proven to be an effective treatment option for
patients with various types of cancer, it isn’t cheap. Unfortunately, insurers
are seemingly more concerned with their own bottom line than the well-being of
consumers. In denying coverage for proton therapy, insurance companies may be
acting in bad faith.
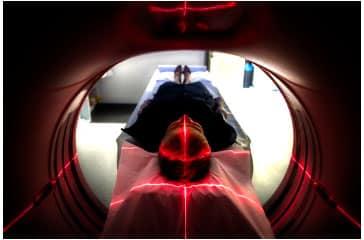
What Is Proton Beam Therapy?
Proton therapy is a type of targeted radiation therapy that is used to treat various types of cancer. It is similar to traditional radiation treatment except that it reduces doses to the healthy heart, lungs, bone, and non-cancerous tissues. This results in fewer side effects and dangerous complications for cancer patients. Proton beam therapy also has more of a direct impact on the tumor, resulting in enhanced tumor control.
Are Cancer Patients at the Mercy of Their Insurers?
Although many insurers cover this alternative cancer treatment, a growing number of people in Nevada are encountering insurance companies that are denying coverage in bad faith. These companies often make unsubstantiated claims about the treatment itself, claim that it is no more effective or safer than traditional radiation therapy or other standard cancer treatments, or assert that proton beam therapy is experimental. In the meantime, insurance denials are costing some cancer patients hundreds of thousands of dollars. For those who can’t afford to pay out of pocket, these bad faith moves may be costing patients their lives.
Why Are Insurance Companies Refusing to Pay?
While insurance companies have offered numerous reasons why these claims denials are legitimate, in the end their decisions are based on expense. Proton therapy is costly. It increases survival rates. It extends the lives of people who are suffering from types of cancer with high mortality rates. And it is less expensive for insurance companies to pay for cheaper treatments and for patients to die sooner. In the end, it’s all about profits before people.
Proton Therapy Denial Lawsuits May Be an Option
Thousands of cancer patients have filed lawsuits against their
insurance companies for denying coverage for proton beam therapy and many
plaintiffs have achieved successful outcomes. Filing a bad faith insurance lawsuit often results in
significant recovery.
When doctors prescribe a treatment plan that is widely accepted throughout the medical community and an insurance company denies the patient the ability to receive that treatment to protect its own profits, it typically doesn’t sit well with jurors. In one recent case, jurors found that the insurer “recklessly disregarded its duty to deal fairly and act in good faith with the (victims).” Fortunately for people who are suffering from cancer and have been denied proton beam therapy, this type of courtroom verdict is common. Sadly, for some it may come too late.









